Support in Insurance Claim
No-Cost EMI
Without Admission
Short Hospital Stay
4.9 Rating on Google
Benefits

Early Detection & Treatment

Reduces Risk of Stroke

Enhances Brain Blood Flow

Supports Faster Recovery
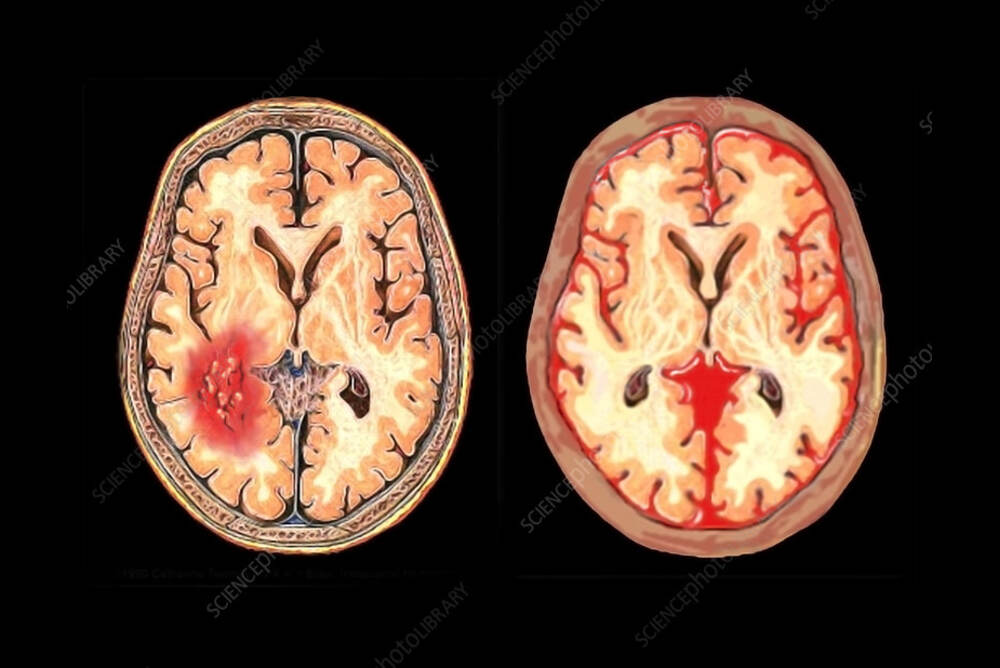
What is Vasospasm in SAH?
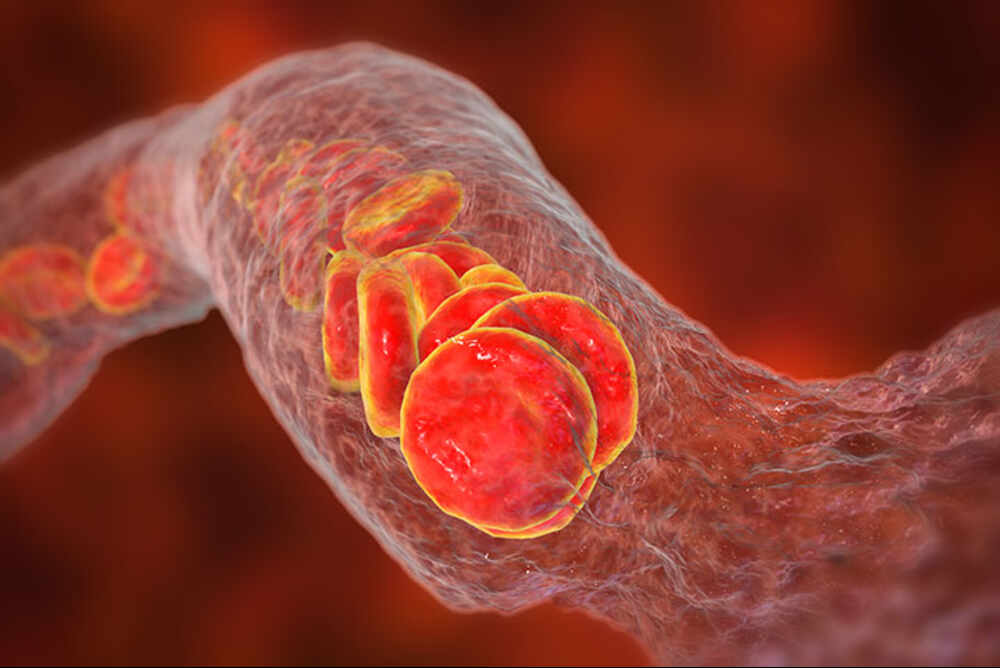
Vasospasm can be a very serious and frequent complication that may be seen following a subarachnoid hemorrhage (SAH). It's the sudden and involuntary shrinking (constriction) in cerebral blood vessels. The narrowing significantly reduces circulation of blood towards the crucial regions of the brain. This results in and thereby denying the brain being denied oxygen and nutrients. This could result in cerebral ischemia or a stroke, which could result in additional brain injury that goes in addition to the first bleeding. Vasospasm typically manifests in an exact timeframe, which is generally between days 3-14 following the hemorrhage. It is an essential aspect to consider in SAH treatment because it is an important cause of death and morbidity in patients who can recover from the initial hemorrhage. A blood vessel in the subarachnoid artery triggers an inflammation response, which irritates the walls of the vessels, increasing the possibility of developing this ailment.
Causes and Risk Factors for SAH Vasospasm
The main reason for vasospasms is an underlying degrading of blood vessels in the subarachnoid space following hemorrhage. As blood clots dissolve they release inflammatory chemicals and other products such as the oxyhemoglobin. These chemicals trigger a chain of events which result in chronic inflammation, irritation, and eventually the continuous contracting of the smooth muscles in the arterial walls. This results in vasospasm.
Many factors could affect the likelihood and severity of this type of ailment:
- Amount of blood: A larger amount of blood seen on the CT scan (often classified with Fisher scales or Modified Fisher scales) is strongly linked to the risk of having severe vasospasm.
- The location of blood Clots that are located close to major arteries in the middle of the brain (like that of the Circle of Willis) poses a higher risk.
- Clinical patients with an earlier neurological diagnosis that is worse (e.g., Hunt and Hess scale) are at greater risk.
- Additional Factors Though the blood itself is the major cause but other elements, like genetic predispositions and certain inflammatory systemic responses, could contribute to the development of these subarachnoid blood haemorrhage complications.
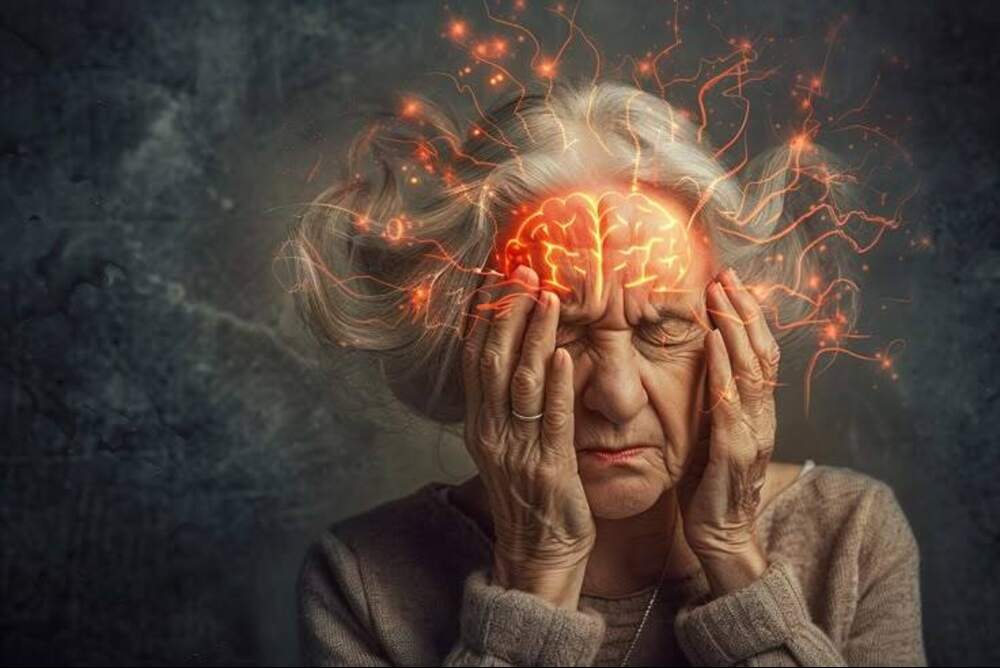
Symptoms of Vasospasm After SAH
Being aware of the signs of vasospasm can be crucial to prompt intervention. Symptoms usually manifest between the days of 3 and 14 following the hemorrhage that caused it, which is often referred to as"the "vasospasm timeframe." Some of the symptoms to be on the lookout for are:
- The state of mind can be altered or confused—situation: Increased drowsiness, anxiety or disorientation.
- Apathy or paralysis: Often affecting one side of the body (e.g. arm, face or leg).
- Speech problems: Slurred speech or difficulty in locating words.
- Headache severe: An abrupt, increasing headache that is distinct from the bleeding that started.
- Seizures:The first time that seizures occur in an individual who didn't suffer from them before.
- Visual disturbances: Blurred vision, double vision, or temporary vision loss.
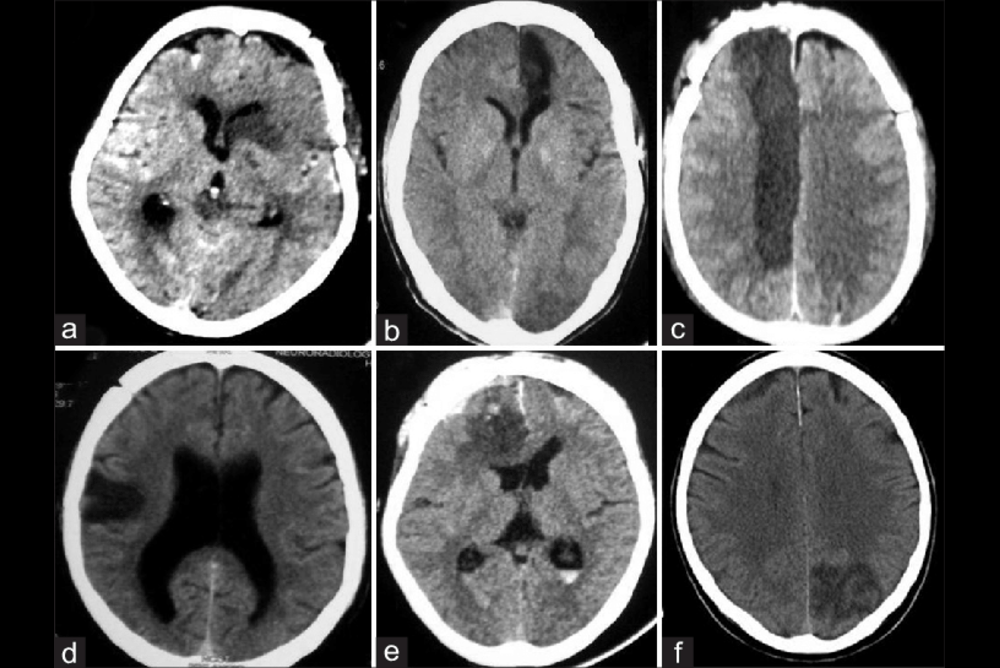
Diagnosis of SAH Vasospasm
At IRFacilities, led by Dr Sandeep Sharma, we use a multi-faceted method to detect vasospasm before it develops into an issue which is a critical aspect in the effective diagnosis for SAH disease. This includes:
- Evaluation of the neurologic state: Frequent checks of motor function, mental state and speech, to detect any signs of decline.
- Transcranial Doppler (TCD) Ultrasound:A non-invasive test that measures the speed of blood flow within the brain's arteries. A faster speed is a sign of the vessel is narrowing.
- CT Angiography (CTA): Provides high-quality images of blood vessels in order to identify the areas of constriction.
- Digital Subtraction Angiography (DSA): The gold standard test that provides the most accurate picture of blood vessels in the brain. It is also utilized to aid later treatment.
- Perfusion CT/MRI: The latest imaging methods allow for the measurement of the flow of blood in various brain regions, and allow for the early detection of a decrease in perfusion caused by vasospasm.
- Biomarker Analysis: Cerebrospinal and blood fluid biomarkers are often assessed to determine patients who are at a higher chance of suffering from vasospasm due to SAH disease.
The Flow Diverter placement technique is the current standard for cases with complex structures. A flow diverter stent can be used to repair the damaged artery. It's not invasive at all and helps the body's natural healing processes, resulting in an effective and long-lasting solution for a variety of aneurysms that are difficult to heal at IRFacilities.
Management and Treatment Options for Vasospasm
The management of cerebral vasospasm requires preventive measures, prompt detection and swift treatment. At IRFacilities under Dr Sandeep Sharma, we follow an established protocol for supporting patients suffering from the subarachnoid hemorrhage (SAH).
Preventive Therapy
The primary preventive drug is nimodipine orally, which aids in recovery. Also, we must maintain an adequate fluid balance to avoid overload and dehydration. In the case of high-risk patients, it is possible to use induced hypertension therapy to increase blood flow. This is done with attentive monitoring to avoid adverse effects
Monitoring and Detection
We make use of sophisticated tools to detect vasospasm in its early stages:
- Transcranial Doppler (TCD) to measure blood flow.
- Continuous EEG to detect subtle brain changes.
- Perfusion imaging is a thorough method for the assessment of blood flow.
Endovascular Treatments
If medical care isn't enough, our team can perform:
- Infusion of vasodilator intra-arterial (verapamil or nicardipine, milrinone).
- Balloon angioplasty to reopen narrowed vessels.
Our Approach
Through combining neurocritical care with advanced therapies, we design customised treatment plans that improve the brain's circulation and enhance outcomes.

Prognosis and Recovery
The prognosis for patients suffering from the subarachnoid hemorrhage (SAH) as well as vasospasm may differ. It's mostly based on the degree of the initial bleeding and how fast treatment is initiated and how quickly vasospasm can be diagnosed, and how the patient reacts to therapy.
Although vasospasm could cause additional brain injuries, early and specialized treatment at IRFacilities, led by Dr Sandeep Sharma, can greatly improve the chance of recovery.
The healing process following SAH is typically the result of a step-by-step procedure. Patients may require:
- Hospital care for stabilisation.
- Rehab programs in the early recovery phase.
- Long-term treatments like occupational, physical, and speech therapy, to restore independence.
The aim is to enhance the quality of life, independence and the quality of living. A solid group of specialists is crucial in guiding patients on this process and ensuring most optimal long-term outcomes.











